PCOS Ultrasound: How to Prepare and What to Expect

Polycystic ovarian syndrome (PCOS) is a medical condition that affects approximately 13% of patients assigned female at birth (AFAB). Because much is still unknown about the disease, diagnosing it can be complex. This article will cover the use of ultrasounds and other tests that help diagnose PCOS and what to expect during an imaging appointment.
While this article provides helpful information, if you have PCOS, your doctor will share your results officially during a follow-up appointment or phone call. However, if you’d like early access to your ultrasound results, PocketHealth offers secure, instant access to your report when it is available. This allows you to review the findings before your follow-up appointment and prepare any questions in advance.
What is polycystic ovarian syndrome (PCOS)?
Though much is still being discovered about PCOS, it is known to be a metabolic and hormonal condition that can develop after puberty. It affects menstruation and menstrual regularity, leads to an excess of ovarian follicles, may reduce ovulation and results in excess androgen hormones. Androgens are medically termed “male” sex hormones, such as testosterone. Everyone, regardless of gender or sex, has both “male” and “female” sex hormones. However, when there is an imbalance in these reproductive hormones, such as with PCOS, it can cause the symptoms mentioned above.
Due to these reproductive and hormonal issues, infertility can occur, which is a common secondary condition. Additionally, it may cause other conditions, such as diabetes or metabolic issues. PCOS currently has no cure, but there are various treatments to help patients manage the disease. Some patients experience varying severity of symptoms, meaning the disease may present itself or be experienced in multiple ways, differing with individual cases. Meanwhile, it continues to be studied and treatments continue to evolve.
Antral follicles vs ovarian cysts
Another aspect of PCOS is the possibility of having excess follicles on the ovaries, called antral follicles. Many people use the term “cysts” interchangeably with antral follicles, but while they are similar, they are not quite the same. As a result, the name “polycystic ovarian syndrome” can be a bit misleading. A follicle is a tiny, fluid-filled sac within the ovary that typically measures 2-9 mm and contains an immature egg. In AFAB patients, multiple follicles develop, with one typically releasing an immature egg during ovulation.
PCOS patients often do not experience ovulation as frequently as is typical. As a result, they may have more follicles than most people, since these follicles do not develop enough to release the egg and dissolve as they should. Instead, the follicles remain on the ovaries, which is a key indicator of the condition.
When a follicle doesn’t release an egg but continues to grow, it can become a fluid-filled sac known as an ovarian cyst. Alternatively, if the follicle doesn’t grow but still doesn’t release the egg, it can resemble a cyst without technically being one. This is the case with PCOS. Despite the name, many patients with PCOS don’t actually have cysts, though some may have both. Instead, they may have numerous follicles that resemble cysts. There has been significant discussion within the medical community about renaming the condition due to this confusion.
What are the symptoms of PCOS?
The most common symptoms of PCOS include:
- Hirsutism: Abnormal hair growth on the patient’s abdomen, chest, face or other areas.
- Weight gain: This is especially common in the abdomen area.
- Irregular menstruation: This may cause periods to skip cycles, come too frequently or even stop completely. It may also cause abnormally heavy bleeding.
- Acne: Acne can be a sign of PCOS.
- Thinning hair: This could be overall thinning or mimic male-pattern baldness.
- Infertility: Menstrual and ovulation irregularities can affect fertility and make conception more difficult.
- Skin tags: These are small skin growths that resemble a bump or wart, often found in the neck or armpit region for PCOS patients.
- Abnormally dark patches of skin: Areas of skin darker than surrounding areas may be seen around the groin, armpits, neck and beneath the breasts.
While many of these symptoms can be a sign of PCOS, it’s helpful to remember there are numerous other possible causes. Bringing these up with a doctor may be a good idea to help rule out various conditions, but many patients may experience these as a normal aspect of their health without any underlying cause or condition.
What causes PCOS?
A singular cause of PCOS has yet to be pinpointed, but there are some linked factors. Patients are more likely to develop this condition if:
- They have insulin resistance: Insulin is how the body processes sugar. When the body is unable to process it normally, it can increase blood sugar, which may cause the ovaries to respond by producing excess hormones. These hormones can lead to weight gain, acne and irregular hair growth.
- Higher androgen levels: When these levels are imbalanced, it can affect ovulation, which is when the ovaries grow and release an egg for reproduction. This reduced ovulation can also cause the ovaries to form multiple follicles, which are small sacs filled with fluid and an immature egg.
- Family history of the disease: When other family members have had PCOS, the likelihood is higher for the patient.
- Chronic inflammation: There is a strong link between long-term inflammation and PCOS. Doctors can evaluate this inflammation by measuring the patient’s white blood cells and C-reactive proteins. These markers can indicate inflammation.
What three symptoms are needed for a PCOS diagnosis?
Patients may experience some symptoms of PCOS for unrelated reasons, meaning other medical conditions may mimic PCOS. For this reason, and because there is a great deal of variation in patients’ experiences, there are some qualifiers for being officially diagnosed with this disease. Patients must experience at least two of the following three criteria:
- High androgen levels: These reproductive hormone levels can be measured through blood tests.
- Irregular or missing menstrual cycles: This criteria includes having 8 or fewer periods within a year. However, many PCOS patients have regular cycles, so this may not always apply.
- Follicles: If multiple follicles are seen on the patient’s ovaries via pelvic ultrasound, this can be a sign of PCOS. Some diagnostic criteria require at least 12 follicles, but there are exceptions to this requirement, and not all patients will meet this prerequisite despite having the disease.
Diagnosing PCOS with an ultrasound
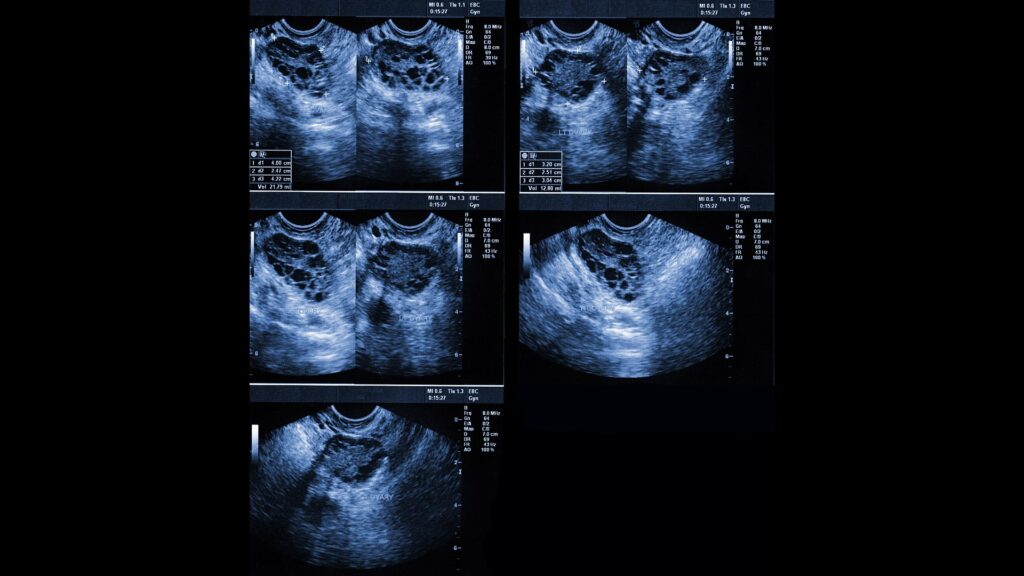
Ultrasound of polycystic ovaries
Because multiple ovarian follicles can be an important indicator of the disease, ultrasounds are a standard tool in helping physicians make a diagnosis. Here is an overview of how ultrasounds work as well as what to expect.
What is an ultrasound?
Ultrasounds use high-frequency sound waves to create internal images. These sound waves are produced by a hand-held device called a transducer, which can be directed to specific areas for assessment, such as the ovaries. As the sound waves bounce off internal structures and organs, they generate an image that can be stored and analyzed later.
What is a transvaginal ultrasound?
Depending on the area to be assessed, ultrasounds can be external, such as with an abdominal ultrasound where the transducer is moved across the abdomen, or internal, such as with a transvaginal ultrasound. A transvaginal ultrasound involves inserting the transducer into the vagina to achieve clearer imaging. PCOS patients may undergo both types of ultrasounds if recommended by their provider, allowing for thorough imaging from multiple angles.
How is a PCOS ultrasound performed?
If the patient is having both an external and internal ultrasound (which is common), here’s what to expect:
- For abdominal ultrasounds, many patients are asked to arrive with a full bladder, as this can improve the conduction of the sound waves and help tilt organs into better positions for clearer views.
- During the abdominal portion of the exam, the patient will lie on their back on the exam table. The abdomen will be accessed, and a conductive gel will be applied. The ultrasound technician will move the transducer across the abdomen, capturing images on a computer as specific angles are achieved.
- After the abdominal portion (if applicable), the patient will be asked to empty their bladder and return for the internal portion of the scan, changing into a hospital gown in preparation.
- The patient will lie on the exam table, and the transducer will be covered with gel before vaginal insertion. Images of the ovaries will be captured from this position, similar to the abdominal portion.
- Once the exam is complete, the patient can return to their usual routine.
How to prepare for a PCOS ultrasound
Here are some tips for preparing for an ultrasound appointment:
- Double-check any preparation instructions: It’s helpful to review any preparation requirements beforehand, such as whether arriving with a full bladder is necessary.
- Bring your requisition or ultrasound form: While the imaging facility may already have your forms, bringing your paperwork may save check-in time if they don’t have it on hand.
- Bring your health card or insurance card: Many clinics require a health or insurance card. A photo I.D. is also commonly needed for check-in.
- Wear comfortable clothes: Wearing something that allows easy access to the abdomen can make the external portion of the ultrasound easier. Also, wearing clothes that are easy to change in and out of is helpful when transitioning into a hospital gown.
Getting my results
Here is some information regarding what to expect with PCOS ultrasound results.
Who interprets my results?
Medical imaging of all types is generally interpreted by a radiologist, a physician who specializes in evaluating medical scans. If applicable, they may compare current scans to past ones, if available, to make comparisons or look for changes. In the case of PCOS, the referring provider may also give input on the results based on the patient’s medical history and other tests. Since this condition affects multiple aspects of health, PCOS care may involve specialists such as endocrinologists, gynecologists or other relevant professionals.
When will I get my results?
Turnaround times for ultrasound results can vary widely depending on the facility and your doctor’s availability. Often, patients wait a week or more and receive their results during a follow-up appointment. With PocketHealth, you don’t have to wait as long—your results are securely accessible as soon as they’re available, allowing you to review them often before your follow-up visit.
Understanding my results
Your physician will provide your results at your follow-up appointment or phone call. For those with early access to their records, it may be helpful to review it in advance so that they can prepare questions ahead of time. It’s common to find medical terminology somewhat confusing, but Report Reader helps you to better understand your report by offering clear, straightforward definitions for medical terms—simply tap or click on any underlined words to reveal their meaning.
PocketHealth also helps patients connect with their results by automatically identifying the organs and bones within their scans. AI-powered anatomical visualization is integrated into the imaging records, enhancing understanding and clarity.
For patients seeking to understand their ultrasound results, this section will briefly cover common terminology found in these types of scans. That said, your medical provider will provide any official interpretations of your results.
Normal Results
If your ultrasound results are normal, you might see terminology in your report such as:
- Unremarkable
- No abnormalities found
- No abnormalities detected
- No ovarian cysts
It may also indicate that the number of follicles is as expected. However, keep in mind that some patients with PCOS may not show abnormalities in follicle count or cysts. This is just one of three possible criteria. If it hasn’t been done already, your doctor may recommend blood work to assess androgen levels.
Abnormal results
Historically, diagnosing polycystic ovaries required the presence of 12 or more antral follicles. Some doctors consider this number outdated, as advancements in ultrasound technology have made it easier to detect follicles, potentially normalizing this count. As a result, some specialists suggest that the number of follicles required for diagnosis should be higher. Your doctor will likely consider your results alongside other factors, such as androgen levels, before making a definitive diagnosis. You may want to ask them if they have specific parameters or diagnostic markers they use, as these can vary.
Here are some examples of abnormal PCOS ultrasound results:
- A higher-than-expected number of antral follicles, which may form a cluster resembling a “string of pearls”
- Multiple ovarian cysts (though this can also indicate other conditions)
- An enlarged ovary or ovaries
- Thicker ovaries than expected
How is PCOS treated?
There are several treatment options, which may vary depending on the symptoms a patient experiences and their personal goals, such as improving fertility. Here are some common treatment types, often used in combination:
- Menstrual regulation: This is typically achieved with hormonal birth control, which can restore regular cycles and may also help with other hormonal side effects, such as acne and excess hair growth.
- Fertility treatments: These can include medications to improve ovulation or in vitro fertilization (IVF). Additional discussions of fertility will be mentioned next in this article.
- Medications for diabetes: Since many PCOS patients are at a higher risk for developing Type 2 diabetes, medications to lower insulin levels are commonly prescribed. These may also help reduce androgen hormones.
- Medications to lower androgens: Drugs that block androgens may help manage side effects like hair loss and facial hair.
- Lifestyle changes: This can include exercise, healthy nutrition or following an anti-inflammatory diet.
PCOS and fertility
Polycystic ovarian syndrome is one of the leading causes of infertility, which has led to increased research on the condition. PCOS can also cause complications during pregnancy, which is why finding an obstetrician experienced with this condition can be helpful. They can evaluate and treat pregnancy complications such as:
- Preeclampsia and high blood pressure complications
- Gestational diabetes
- Higher rates of C-sections due to complications
- Preterm labor (before 37 weeks gestation)
Despite these elevated risks, many patients with PCOS have healthy pregnancies and are able to conceive with little or no medical intervention. Others may require fertility medications or in vitro fertilization. While the process may seem stressful, many fertility specialists have extensive experience helping PCOS patients get pregnant and have healthy deliveries. If you’re interested in conceiving, you may want to consider asking your doctor for recommendations for fertility specialists or obstetricians experienced with PCOS pregnancies.
Frequently asked questions
Here are some commonly asked questions regarding PCOS.
Does having PCOS put me at risk for other health conditions?
According to the CDC, there are several health conditions that individuals with PCOS may be at a higher risk of developing due to the higher prevalence of metabolic syndrome often associated with the condition. However, many of these risks can be reduced or managed with proper treatment for PCOS. Here are some to be aware of:
- High blood pressure and LDL cholesterol: The metabolic effects of PCOS can influence blood pressure and cholesterol levels.
- Sleep apnea: This condition causes interruptions in breathing during sleep. It is highly treatable through therapies like continuous positive airway pressure (CPAP) devices or other treatments.
- Heart disease: Metabolic syndrome increases the risk of heart disease in those with PCOS.
- Diabetes: The likelihood of developing Type 2 diabetes is higher in individuals with PCOS. Fortunately, treatments for diabetes, such as medications like metformin, can also help manage PCOS symptoms by improving insulin resistance.
What is the difference between PCOS and endometriosis?
Because both of these conditions affect AFAB patients and can impact menstruation and fertility, they are often confused with each other. However, they are quite different. PCOS occurs due to an excess of androgen hormones and other factors, whereas endometriosis is when cells from the uterine lining (endometrium) grow outside the uterus, such as on the ovaries, fallopian tubes and other areas. Endometriosis causes painful periods, scar tissue formation and other factors that can lead to fertility challenges. Fortunately, there are specialists for endometriosis, just as there are for PCOS, who can help patients navigate treatment and fertility options.
Will PCOS go away with menopause?
The metabolic and hormonal symptoms of PCOS do not go away with menopause, even if menstrual issues are alleviated. Ongoing treatment throughout the patient’s lifetime is generally recommended to manage the symptoms and effects of polycystic ovarian syndrome. Proper medical management can significantly improve the patient’s quality of life and overall health.
Can I have PCOS without symptoms?
Yes, some patients have mild or no noticeable PCOS symptoms. As time progresses, some may start to experience outward symptoms, but some don’t realize they have PCOS until they encounter issues like unexplained weight gain or difficulty conceiving.
Take control of your health journey
PocketHealth makes it simple to keep track of your ultrasound reports and other diagnostic imaging records. All of your imaging results can be accessed online anytime. If needed, reports can also be easily shared with other physicians in your care team, including PCOS specialists. When used in conjunction with your medical provider’s professional advice, it is a powerful tool for organizing and understanding your imaging results and your health.
Another tool PocketHealth provides is MyCare Navigator, which gives personalized insights to your health and identifies any recommended follow-up steps. This feature can also generate personalized questions to ask your doctor based on the findings in your report, ensuring you make the most of your consultation.
Published: March 11, 2025
Trusted by more than 800+ hospitals and clinics.