Breast Cancer Risk Assessment: What to Know and Expect

A breast cancer risk assessment is a way to evaluate potential factors that may predispose you to developing this disease. Some of these factors are based on your family history or genetics and others on lifestyle behaviors. Your physician can then use this assessment to take preventative measures, such as increasing breast cancer screenings or helping you maintain healthy habits. This guide will discuss the specific risk factors in these assessments, the limitations and strengths of these tools and how physicians use the results to create individualized care plans.
What is breast cancer risk assessment?
There are currently 24 breast cancer risk assessment tools available, many of which are similar in execution. Typically, you answer a short series of questions and receive an automated score based on your responses. Completing the questions usually only takes 5-10 minutes. They cover aspects of your health history, age and other factors. Individual risk factors will be discussed further in this guide.
It’s important to remember that these assessments only estimate the likelihood of your developing breast cancer. High probability doesn’t mean you will get the disease, just as low probability doesn’t guarantee you won’t develop it someday. Your breast cancer risk assessment score isn’t meant to cause you panic or stress. It is a way to help you and your doctor decide if you should take precautions and protective measures.
PocketHealth’s breast health tools provide patients with personalized breast cancer risk assessments and simplified mammogram management. Designed to increase early detection of breast cancer, these tools enable patients to take control of their breast health. Learn more about PocketHealth’s breast health tools here.

Breast cancer risk factors
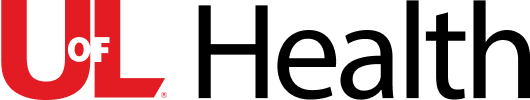
Current statistics estimate that 12% of people assigned female at birth (AFAB) will develop breast cancer within their lifetime. While those assigned male at birth can also have breast cancer, their likelihood is considerably lower. Consequently, risk factor assessments are specifically designed for AFAB individuals. Here are some of the risk factors taken into account when determining your breast cancer risk assessment score.
Age
Your chances of developing breast cancer increases with age. For this reason, many doctors recommend AFAB people with average risk should have their first mammogram around the age of forty, repeating it every one to two years as directed.
Here are some statistics of your risk of breast cancer by age and the chances of it developing within the next 10 years:
- Age 40: 1 in 69
- Age 50: 1 in 43
- Age 60: 1 in 29
- Age 70: 1 in 26
Family history
Though many people with breast cancer have no family history of the condition, having family members who have had it can increase your risk. First-degree relatives, such as a sister, mother or daughter can nearly double your own risk. If you have two first-degree relatives with this condition, that risk is tripled. Having a brother or father with a history of breast cancer also affects your chances.
Having a previous history with breast cancer
If you’ve had breast cancer before, you have a higher chance of developing a new breast cancer, either in the same or opposite breast. This is known as a secondary primary breast cancer diagnosis, as these are different cancer cells, not the same ones from the original diagnosis. It may appear in the other breast, in a different part of the same breast, or as a completely different type of breast cancer. Fortunately, the risk is estimated at around 18%.
A recurrence of the same, previous cancer is also a possibility. This occurs when some of the original cancer cells survive in your body, multiplying and returning as the same cancer. This is different from a completely new diagnosis. The most common timeframe for recurrence is within 3 to 5 years of your initial treatment. Factors that influence recurrence include the type of treatment you received, the stage of cancer at diagnosis, whether it had spread to other areas, etc. Here are some statistics to be aware of:
- If you’ve had a lumpectomy and radiation therapy, you have a 3 to 15% chance of the cancer recurring within 10 years
- If you’ve had a mastectomy, you have a 6% chance of recurrence within 5 years
- If your previous breast cancer spread to your axillary lymph nodes (located in the armpit region), the risk of cancer recurrence is 25%
Having dense breast tissue
Patients with dense breasts have an increased risk of breast cancer. This happens when breasts have less fatty tissue and more fibrous and glandular tissue. It also makes it harder to detect cancer via mammograms. This is a common condition as nearly half of AFAB people 40 and older have dense breast tissue. For those with very dense breasts, breast cancer rates increase by 4 to 5 times in comparison to those with fatty breasts. Here is how breast density is officially categorized:
- Entirely fatty breast tissue: Only 10% of AFAB people have nearly all fatty breast tissue
- Scattered fibroglandular breast tissue: Nearly 40% of AFAB people belong in this category. Breasts have some dense areas of fibrous connective and glandular tissue but the majority is still fatty tissue
- Heterogeneously dense breast tissue: Nearly 40% of AFAB people have some fatty tissue but several dense areas of fibrous connective and glandular tissue. This is categorized as dense
- Extremely dense breast tissue: Around 10% of AFAB people have nearly all dense fibrous connective and glandular tissue. It is also categorized as dense and has the highest risk factor for breast cancer
Factors that affect breast density can include:
- Genetic predisposition
- Those who use menopausal hormone therapy
- Those with a lower body mass index
- Those who have had children have a lower rate of breast density
- Aging can make breasts more fatty and decrease density
Genetic mutations
There are several genetic conditions that can increase the likelihood of breast and other cancers. The most common genes associated with this risk are the BRCA1 and BRCA2 genes. In their healthy forms, they help repair damaged DNA. However, mutated versions can lead to abnormal cell growth and potentially result in breast cancer. These mutations are hereditary and can be passed down. Here is some data on how these conditions increase your risk:
- Those with these mutated genes have a 70% chance of developing breast cancer by the age of 80
- AFAB people with these mutations have a higher chance of developing breast cancer at a younger age or to get it in both breasts
- Assigned male at birth people with these mutations have a higher risk of breast cancer
- 1 in 40 Ashkenazi Jewish people in the U.S. have these mutations, though any ethnicity can have them
Menstrual factors
Long exposure to the hormones progesterone and estrogen throughout your life is an important breast cancer risk factor. If you had your first menstrual cycle before the age of 11, your risk increases by 15 to 20 percent due to longer-than-typical hormone exposure. Similarly, starting menopause after age 55 is associated with a higher risk, rising by 3% each year.
Reproductive factors
Not having children results in increased lifetime estrogen exposure, raising your chances of developing breast cancer. However, having your first child after the age of 35 may also increase your risk. This is because breast cells grow rapidly during pregnancy, so if there are problematic cells, they can be copied during this process. The more genetically damaged cells present, the more likely they are to turn into cancer. As a person ages, they are more likely to have these damaged cells, which is why age and pregnancy can be correlated with cancer risk.
Previous radiation exposure
Being exposed to chest radiation in the past (likely from previous treatment for cancer or other conditions) can increase your chances of developing breast cancer by as much as 3 to 7 times. The younger the person was during the initial radiation treatment, the higher their risk, as the breasts may have still been developing if they were a teenager or young adult. Radiation received after age 40, however, doesn’t seem to carry the same risks.
Race and ethnicity
Certain races are more prone to breast cancer than others, though it is unclear as to why. The overall risk percentage for those AFAB in the U.S. is at a 12% baseline. Here are some statistics based on race:
- Non-Hispanic white: 14%
- Non-Hispanic Black: 12%
- Non-Hispanic Asian and Pacific Islander: 12%
- Hispanic: 11%
- Non-Hispanic Native American: 10%
One thing to note, despite most breast cancer types being more prevalent among Caucasian people, a less common type called triple-negative breast cancer is nearly three times more prevalent among Black people who are AFAB. While this cancer makes up only 10-15% of all breast cancers, it is particularly invasive, aggressive, and more difficult to treat.
Lifestyle factors
Unlike previous factors, lifestyle decisions give you more control over your risk levels. Here are some lifestyle habits that play a role in the possible development of breast cancer:
- Food habits: Eating high quantities of saturated and animal fats can greatly increase breast cancer risks. One study found a nearly 50% increase with patients who ate a diet heavy in such fats. In contrast, a diet rich in fruits and vegetables can reduce the likelihood of developing breast cancer.
- Drinking alcohol: Drinking too much alcohol is another risk factor. Those who have 2-3 alcoholic drinks per day increase their risk by 20%.
- Exercise: Being sedentary or overweight increases the risk of breast cancer. Regular moderate to vigorous physical activity can lower this risk by up to 25%. Staying active boosts your immune system’s ability to fight cancer cells, and maintaining a healthy weight reduces blood estrogen levels, which are linked to breast cancer development.
- Hormone replacement therapy (HRT): HRT is commonly used to alleviate menopause symptoms like hot flashes. While estrogen alone doesn’t have the same link to breast cancer as a combined regimen of estrogen and progestin, the duration of HRT use is important, as risks increase over time. Fortunately, the increase in breast cancer rates due to HRT is relatively low. For every 10,000 people taking HRT for one year, there are only about 8 additional cases of breast cancer.
- Smoking: Smoking for over 10 years increases breast cancer risk by about 10%, whereas shorter-term smokers and non-smokers do not face the same increase.
Limitations of risk assessment calculators
Breast cancer risk assessment tools are valuable for calculating your risk of developing the condition. However, they are not perfect and should be used alongside professional medical advice to gain a more accurate understanding of your health. Often, this means they will recommend getting a mammogram to provide additional data for review. Here are some limitations of these risk calculators to be aware of:
- Doesn’t always factor race or ethnicity: Certain races have slightly higher or lower cancer rates and not every risk calculator reflects this
- Doesn’t always factor those with BRCA1 or BRCA2 mutations: Some assessments don’t always ask about genetic conditions that predispose one to cancer
- Several risk factors are not included: Depending on the type of calculator used, certain risk factors may not be assessed
- Can’t actually predict if you’ll get cancer: Calculators assess risk only, they can’t definitively state that you will or won’t develop breast cancer
- Doesn’t always factor personal cancer history: Many calculators don’t take into account if you’ve had cancer previously, which is a big factor for getting it again
Breast cancer risk assessment tools
There are multiple assessment models, some of which are considered more helpful than others. Here is a quick review of the more prevalent breast cancer risk calculators:
Gail model (BCRAT)
The Breast Cancer Risk Assessment Tool (BRCAT) is commonly called the Gail model, after Dr. Mitchell Gail, who created it while working at the National Cancer Institute. It is the most widely used of all the assessment methods in the medical industry and takes only minutes to complete.
This assessment tool estimates a person’s risk of developing breast cancer within the next 5 years and throughout their lifetime, using health and personal data as factors. Clinicians and medical providers favor the Gail model over other types due to its simplicity, speed, and ability to collect crucial information that helps estimate risk and determine if precautions should be taken.Here are some of the risks it measures:
- Race/ethnicity
- Age
- Age of your first menstrual cycle
- If you have a family history of breast cancer
- When/if you had children
- Previous breast biopsies
Not intended for: The Gail model incorporates data for Asian and Pacific Islander patients as well as Black, Hispanic and Caucasian patients. It is still lacking data for other racial and ethnic groups.
Other risk assessment models
Besides the Gail model, there are multiple other risk assessments available to patients and providers. They all have their uses and benefits, though there are limitations as well. Here are the current models used in the health industry:
- IBIS (Tyrer-Cuzik model): This model is one of the most comprehensive in terms of collected risk factors
- Breast Cancer Surveillance Consortium’s (BCSC) Risk Calculator: This model additionally factors the chances of breast cancer spreading to other parts of the body
- BRCAPRO: This model has a focus on genetic mutations of the BRCA1 and BRCA2 genes
Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm (BOADICEA): This model assesses risks for both breast and ovarian cancer - Black Women’s Health Study (BWHS) Breast Cancer Risk Calculator: This model focuses on Black patients and their specific risk factors, including the higher prevalence of triple-negative breast cancer
Getting your results

If you’re taking an assessment by itself, you’ll often get your breast cancer risk assessment score instantly, especially if it is taken online. However, many of these methods are used in combination with a mammogram, which improves estimate accuracy. Mammogram results can take up to one or two weeks, depending on the imaging facility, but with PocketHealth, you can see your mammogram images and report, often as soon as they’re released by the radiologist.
Discuss the results with your doctor
Discussing assessment results with your medical provider will help you plan any next steps that may need to be taken. If you’ve taken a risk assessment and a mammogram, they will likely suggest a follow-up appointment to review everything. For patients who have had a mammogram, preparing questions in advance can make the next appointment more productive. PocketHealth’s MyCare Navigator can suggest personalized questions to bring up with your doctor based on your finalized mammogram report.
What are the next steps?
Next steps will depend on your assessment results. If you have a score indicating a higher risk for developing breast cancer, your doctor may suggest earlier or more frequent screenings. Other possibilities include getting tested for genetic mutations, having a mammogram (if you haven’t already), or undergoing additional imaging, such as a breast MRI. Although mammograms are the typical gold standard for imaging, breast MRIs and other techniques may provide additional details not shown on a standard mammogram.
If you are deemed at very high risk for breast cancer, more aggressive treatments may be considered. This could include prescribing medications that significantly lower cancer rates or even preventative surgeries such as mastectomies. Your doctor will discuss suggestions so you can come up with a plan together.
How accurate are the results?
Breast cancer risk assessments represent population averages and cannot precisely determine which individuals will develop breast cancer. However, they provide a general idea of your risk, which is useful for taking preventative measures such as additional screenings or genetic testing. A high score doesn’t guarantee you will develop breast cancer, just as a low score doesn’t necessarily mean you won’t. Using these assessments in conjunction with mammograms enhances accuracy, making them an important part of a comprehensive approach to breast cancer prevention.
Stay on top of your breast health with PocketHealth
For patients who have had a mammogram along with their risk assessment, PocketHealth offers the advantage of faster, secure access to your completed report. You can view your results immediately after they are uploaded, so you won’t have to wait until your follow-up appointment to see your mammogram. PocketHealth’s Report Reader helps you understand complex medical terms in your report by offering easy-to-understand definitions that you can tap or click on to view. This feature empowers you to engage more confidently in discussions with your physician, giving you greater control over your health journey and ensuring you are well-informed every step of the way.
Published: August 16, 2024
Trusted by more than 800+ hospitals and clinics.