Mammogram: Your Guide to Breast Cancer Screening

Regular mammogram screenings provide important information about your breast health and enable earlier breast cancer detection, improving recovery rates.
Mammogram screening is a valuable tool to assess your breast health, and regularly scheduled mammograms help your doctor catch breast abnormalities that could be cancerous. Finding breast cancer early is critical to the effective treatment of the disease, and regular mammogram screenings can help alert your doctor to new changes in breast tissue.
New draft 2023 mammogram guidelines issued by the U.S. Preventive Services Task Force (USPSTF) suggest that a woman at average risk of breast cancer should receive a mammogram every two years beginning at 40 years old. Recent research indicates that regular mammograms between 40 and 49 years old reduce breast cancer mortality risk by 12-29%.
Some women may be at greater risk and may have mammogram screenings more often. Your doctor may send you for a mammogram as young as 30 years old if you are a carrier of the BRCA1 or BRCA 2 gene or have had radiation to your chest since both factors increase your risk of developing breast cancer.
If it’s time for your mammogram screening you may have questions about the appointment, including:
- How does a mammogram work?
- How can I prepare for my appointment?
- How do I understand my mammogram results?
- What are the next steps after my mammogram appointment?
Understanding how mammograms work and how regular screening benefits you, lets you stay on top of your health and have more informed discussions with your physician about the results.
What is a mammogram?
A mammogram is an X-ray that allows your healthcare team to assess the tissue of your breast for irregularities, including lumps. Mammograms help your doctor investigate any abnormalities you may feel while doing a breast self-exam, but they can also catch lumps too small for you to feel.
Mammograms use X-ray technology to examine breast tissue. While very small amounts of radiation are released during a mammogram, the benefits of catching breast cancer early outweigh the radiation exposure for most. If you have concerns about the impact of the radiation from a mammogram, speak with your doctor to better understand the risks of the procedure.
There are 3 different types of mammograms:
- Standard: images of breast tissue are released on film.
- Digital: images of breast tissue are released onto an electronic file, allowing your doctor to see different views of the breast.
- Digital breast tomosynthesis: also called a 3D mammogram, the screening uses X-rays to create three-dimensional images of the breast.
After your mammogram screening test, the mammography technician will send the images of your screening to a radiologist. A radiologist is a doctor who specializes in diagnosing and treating injuries and diseases using medical imaging. Once a radiologist has assessed your mammogram images, they will send the images and a report to your doctor, who will schedule an appointment to discuss any results. PocketHealth enables patients to access their mammogram results as soon as the radiologist has completed their report. Access your records here.
How often should you get a mammogram screening?
Women with average breast density should begin getting regular mammograms at age 40. New U.S. breast cancer screening guidelines for 2023 state that receiving regular mammograms from age 40 onwards can reduce the risk of serious breast cancer outcomes and mortality.
Breast tissue density is an important factor when considering breast cancer risk and screening. A mammogram can show the radiologist how much dense fibroglandular tissue is in your breasts. Women with very dense breasts, containing a lot of fibroglandular tissue, have an increased risk of developing breast cancer but should still receive regular mammograms. Dense breast tissue can make mammogram screening less effective for young women, so speak to your doctor if you’re concerned you may fall into this category.
7 reasons to get a mammogram
Whether or not you have any signs or symptoms of breast disease, the USPSTF draft recommends a mammogram screening every two years for all women at average risk of breast cancer between the ages of 40 and 74 years of age.
Reasons you should have regular mammogram screenings include:
- Age: the USPSTF mammogram screening guidelines suggest that women between 40 and 74 years of age get regular mammogram screenings every two years. If you are under 40, your doctor may send you for a mammogram if you have breast cancer risk factors.
- Family history of breast cancer: having a first-degree family member (e.g., mother, daughter, or sister) with breast cancer increases your risk, too.
- Other risk factors: certain risk factors make you more likely to develop breast cancer. These risk factors include carrying the BRCA1 or BRCA2 genes or receiving chest radiation.
- Nipple discharge: discharge is sometimes associated with abnormal tissue formation or tumor growth in the breasts. A mammogram can help to determine whether or not nipple discharge is breast cancer-related.
- Lumps in the breast: breast lumps can be benign or malignant (i.e., cancerous). If you or your doctor has noticed a lump during a physical exam, a mammogram can uncover more details about the growth.
- New or worsening pain or discomfort: you should discuss any change in breast health with your doctor, including pain or discomfort. Often breast tumors are painless, but in some cases can cause breast discomfort or pain.
- Finding early-stage cancer: one benefit of screening is that mammograms can help detect very small lumps within the breast tissue that cannot be felt during a self-exam. Detection of these tiny abnormalities allows treatment to begin earlier and increases the likelihood of its effectiveness.
Does a mammogram hurt?
For the technologist to get the clearest images of your breast tissue, the breast must be compressed, which can cause some discomfort. Avoiding a mammogram in the 10-14 days before your menstrual period can help reduce discomfort and if you have a breast condition that makes your breasts sensitive or tender, speak to your doctor about taking pain medication before your appointment.
How effective are mammograms for detecting breast cancer?
Mammogram imaging allows the radiologist to see very small abnormalities in breast tissue, even those too small to feel with a physical exam, and is very effective at screening for breast cancer. Mammograms allow malignant abnormalities to be detected early, increasing the effectiveness of cancer treatment. Research in 2020 shows that mammogram detection of breast cancer early on improves recovery rates and reduces death from breast cancer by 41% over the ten years following detection.
Although regular mammogram screenings can mean cancer is caught early, making treatment more effective, mammograms also have limitations. Some cancers cannot be detected on a mammogram because of the location of the cancer or the density of breast tissue. Mammograms also release a small amount of radiation during imaging, but this low amount does not outweigh the benefits of regular mammograms, according to the National Cancer Institute. If you are concerned about radiation from mammogram screenings, talk to your doctor about the risk to you.
What are false-positive and false-negative results?
Mammograms can give false-positive or false-negative results, meaning the images do not accurately represent what’s happening in your body. With a false-negative result, a mammogram indicates that there are no concerning irregularities in your breast tissue— when there are. On the flip side, a false-positive result indicates there is an area of concern where there isn’t one.
A 10-year research study that false-positive results happen about 12% of the time, but that only 4% of those mammograms indicate a “positive” result in a diagnosis of cancer. The National Cancer Institute states that mammograms give false-negative results, missing cancer that’s present at the time of screening, about 20% of the time.
False-positive and false-negative mammogram results can cause a lot of stress to the patient and lead to unnecessary testing or, in some cases, can cause cancerous results to be missed.
How to prepare for a mammogram screening
A mammogram is an integral part of breast cancer screening and requires only a short appointment, but there are some steps you can take to prepare in advance:
- Bring your requisition form. You’ll be asked for your requisition form when you arrive for your appointment and having it ready and accessible makes checking in for your appointment quicker.
- Use the same clinic. If possible, try to get your mammogram screenings done at the same clinic each time. This can make it easier to compare imaging. If you’re unable to do this, give the mammogram clinic the names and addresses of the clinics where you’ve had mammograms and the dates.
- Schedule your appointment when your breasts aren’t tender. Your breasts may feel sensitive leading up to or during your menstrual cycle, so avoid making your mammogram appointment during these times. Often, breasts are most tender the 7-10 days before your period.
- Avoid deodorant or antiperspirant, as well as lotions. Don’t apply deodorant or antiperspirant on the day of your mammogram appointment, and make sure to wipe off any deodorant residue since the mammogram can pick up the aluminum. Also, avoid using lotions or creams on your breast or the surrounding area that day.
- Remove long earrings or necklaces. It’s best to avoid wearing jewelry to your appointment because the metal can interfere with your images.
- Wear a top and bottom, rather than a dress. You will be asked to remove your top and bra during your mammogram, so wearing pants or a skirt may make you more comfortable during your appointment.
- Reduce caffeine intake. Caffeine can make breast tissue more tender, so try to avoid—or limit—caffeine intake for 4-5 days before your appointment.
- Let the clinic know if you have implants. Breast implants require modifications to the mammogram process, so your appointment may take longer. Also let the technologist know about any changes or sensitive areas, or if you are breastfeeding.
- Obtain prior mammogram imaging. Speak with your doctor to get imaging from previous mammogram clinics so that you can bring the imaging to your new appointment or request that your doctor send the imaging to the clinic prior to your appointment. PocketHealth helps you keep your medical imaging securely organized together, so you can bring them to your appointments yourself or share them at referral appointments. Having all your mammogram imaging in one place lets you easily monitor different imaging results over time.
The imaging clinic or department will provide wipes to clean up after your screening, but you may wish to pack deodorant or antiperspirant to bring with you to wear after the appointment. Also, if you are concerned about pain during your appointment, ask your doctor if over-the-counter medication can help reduce discomfort.
Questions to ask during and after your mammogram screening
During your mammogram appointment, the technologist will go over the procedure with you and outline each step. If you have any questions about the details of the process or what to expect, you can ask for clarification before the screening begins.
During your mammogram appointment, you can also ask:
- How long will the procedure take?
- Can we stop the mammogram if I feel pain or discomfort?
- Can I have a support person in the room with me?
- How long will it take for my doctor to receive my mammogram results?
- Can I receive my results at the same time as my doctor?
After your mammogram appointment, your doctor will schedule a follow-up call or in-person appointment to discuss your results. At this appointment, you can ask any questions about your results, such as:
- What are the next steps? Your doctor may have guidance for you regarding your mammogram results, even if the results do not show malignant irregularities.
- Do I need additional testing? In some cases, your doctor may suggest additional testing, including additional imaging, to explore any irregularities shown on your results.
- What do my results mean for my risk of cancer? Even if your mammogram shows an irregularity in the breast tissue, it does not necessarily mean you have cancer. Many irregularities are benign or low risk.
- When should I get my next mammogram? Depending on your results, your doctor may send you for another mammogram in six months or a year or may recommend you wait the standard two years for your next appointment.
How to access your mammogram screening and report
You may wish to access your mammogram imaging and report as soon as possible. With PocketHealth you can quickly and easily access your mammogram images and report—often before your follow-up appointment with your practitioner.
PocketHealth enables you to securely access, share and store your imaging and other health information in one place, which makes it easy to compare and review images over time.
Mammography terminology can be complicated and you may not comprehend all of the medical terms used in your report. PocketHealth Report Reader makes it easy to understand terms in your mammogram report and also highlights any follow-up recommendations, so you can feel informed and confident when speaking to your doctor at your mammogram follow-up appointment.
“I recently had mammograms taken and was to see my doctor in five weeks to hear the results. PocketHealth gave me the results as soon as they were ready. While my results were clear, PocketHealth gave me peace of mind because, without it, I would have worried for weeks about my results.”
– Mammogram Screening Patient
Understanding your mammogram results
Mammograms can show different areas of irregularities within your breast tissue, not only lumps or masses. Both normal and abnormal mammogram images can show other parts of your breast tissue that aren’t cancerous but may indicate a different health concern or may be completely benign, including cysts, fibroadenomas or calcifications. Here’s a list of common irregularities in breast tissue found by mammograms:
- Tumors are lumps or masses of hard tissue and can be benign or malignant (i.e., cancerous).
- Cysts are fluid-filled masses that are rarely indicative of breast cancer.
- Fibroadenomas are solid, moveable lumps of normal breast tissue cells. These lumps are usually not cancerous, although they can grow in size.
- Calcifications are small, hard pieces of calcium sometimes found in soft breast tissue. Calcifications may be found singly or in clusters.
Normal, abnormal and cancerous mammogram images will show some differences, but all mammograms will have a black background and show the image of the breast in variations of gray and white. In general, denser tissue appears white and less-dense tissue, including fat, appears gray.
Therefore, a normal mammogram image of healthy breast tissue will show primarily dark areas interspersed with some lighter or cloudy-looking areas. Abnormal images may show thicker, light areas of more dense tissue, or smaller light areas of dense tissue, while a mammogram image indicating breast cancer will likely show one or more clearly defined white, opaque masses within the breast tissue.
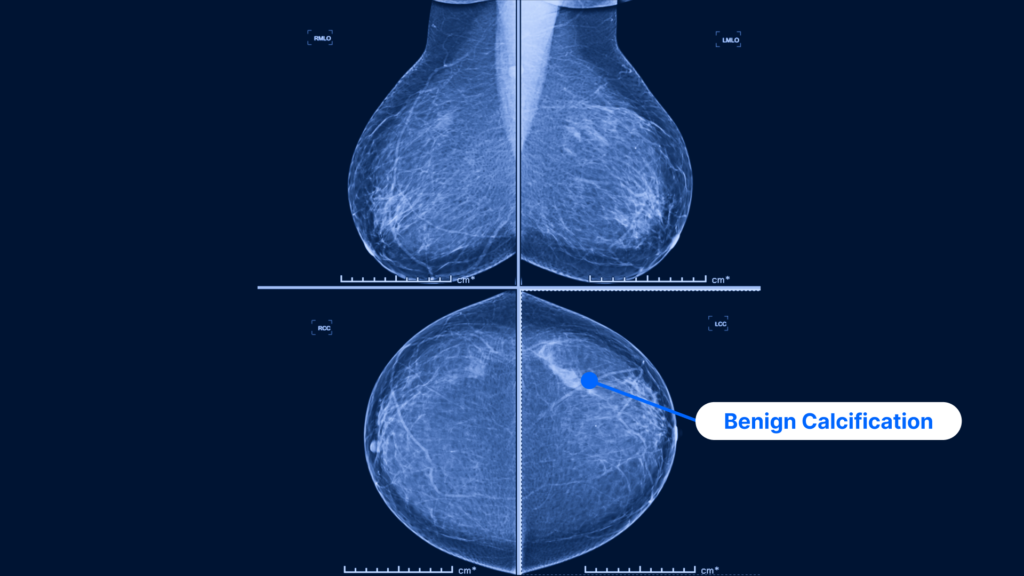
A mammogram image showing two standard views: the MLO view (i.e. taken from the side) is on the top and the CC view (i.e., taken from above) is on the bottom. The CC view of the left breast more clearly shows a benign calcification with no evidence of malignancy, falling into BI-RADS category 2.
What is the Breast Imaging-Reporting and Data System (BI-RADS)?
Created by the American College of Radiology, BI-RADS is used to report the results of every mammogram. The system accounts for the results of the mammogram and recommends follow-up tests, if needed, and indicates the degree of the risk that an abnormality may be cancerous.
BI-RADS works by organizing the results of each mammogram into 7 categories based on cancer risk. Each category is given a number, with lower numbers indicating no risk or benign changes and higher numbers indicating areas of breast cancer concern. A BI-RADS category of “0” indicates an incomplete scan, so additional testing or a repeat mammogram is required.
- Category 0: scan was incomplete or unclear, and you will need further testing, which might include another mammogram for comparison.
- Category 1: a normal test result, considered ‘negative’ in that nothing abnormal or new was detected.
- Category 2: also a negative test result, which includes some sort of non-cancerous finding like a benign calcification.
- Category 3: a possibly benign scan but one which reveals a finding that suggests a follow-up image be taken, generally within the year.
- Category 4: a suspicious finding which is not confirmed to be cancer. A biopsy is often recommended.
- Category 5: these findings typically suggest cancer: a biopsy is strongly recommended.
- Category 6: this category is only used for findings taken after cancer has already been proven.
Depending on the results of your mammogram, your doctor may send you for other breast cancer screenings, including a breast ultrasound, a breast MRI or molecular breast imaging. These tests can be useful in determining whether a lump is a hard mass or a fluid-filled cyst. If cancer has been detected, these additional screenings can indicate how advanced the disease is. In some cases, different breast cancer screenings will be used in conjunction with each other to ensure no cancer has been missed.
Protect your breast health with regular screenings
While breast cancer continues to be one of the most common forms of cancer among women, regular mammogram scans can significantly reduce your risk of serious breast cancer complications. If you’ve missed or delayed a regular mammogram screening, it’s never too late to start or to catch up—early detection of breast cancer can improve treatment outcomes.
If you’re approaching 40, speak with your doctor about regular mammogram screenings and discuss the benefits and limitations of the technology, as well as your cancer risk.
Knowing how a mammogram works, what mammogram images look like, how to access your report and what questions to ask your doctor at your follow-up appointment will help you feel prepared during your appointment and more confident about your breast health.
How PocketHealth works
Learn more about how to use PocketHealth to access and share your mammogram records.
Published: August 30, 2023
Trusted by more than 800+ hospitals and clinics.