A breast cancer diagnosis typically requires a series of specific medical tests and imaging appointments. Several factors are considered to confirm the diagnosis or rule out cancer entirely, which may feel overwhelming for patients who are new to these types of procedures. Remember, although it is understandable to be nervous, try not to panic. Many abnormal findings in breast imaging turn out to be benign. This guide will explain the imaging and other testing methods involved in diagnosing breast cancer, as well as what risk factors to be aware of.
For those looking to take proactive control of their breast health, PocketHealth can help. With secure, easy access to your breast imaging records, PocketHealth allows you to better understand your breast health by offering personalized estimated breast cancer risk scores. This enables you and your doctor to make informed decisions about preventive measures and future screenings.
Breast cancer occurs when cancerous cells in the chest area grow uncontrollably, forming tumors that may spread to other areas, such as lymph nodes or other parts of the body. Most cases of breast cancer affect patients assigned female at birth (AFAB), though, in rare instances, patients assigned male at birth (AMAB) can also be affected. The disease is most common in patients aged 50 or older, though it can develop in younger individuals as well. In the U.S., the likelihood of developing breast cancer is about 1 in 8 for AFAB patients. Fortunately, mortality rates have dropped to 2.5%, with ongoing studies and treatments aimed at further reducing this rate.
In the early stages, breast cancer may not cause noticeable symptoms, which is why routine screenings, such as mammograms, are important. The earlier cancer is detected, the more effective treatment can be.
For cases that do cause symptoms, they may include:
There are multiple types of breast cancer, which may affect treatment plans and methods:
In addition to the main types of breast cancer, there are subtypes that further influence treatment methods. The way the cancer responds to specific hormones, such as progesterone and estrogen, helps categorize these conditions. Hormone receptors found on cancer cells capture hormones from the patient, using them as a fuel source that allows the cancer to grow and spread. Pathology of the cancer will indicate which hormone, if any, it is reacting to. Here are some categories of cancers based on their receptor cell type:
A mammogram scan
Here is a brief overview of how breast cancer diagnosis takes place.
Though not an actual diagnosis, breast changes are a starting point if the patient either finds a lump or abnormality themselves or if it is detected during a breast exam at the doctor’s office. Most breast lumps turn out to be benign, but doctors typically recommend additional testing to confirm.
One of the most common methods for detecting breast cancer is through a screening or diagnostic mammogram. These are X-rays that use low-dose radiation to capture internal images for analysis. During the scan, the breasts are compressed between two plates to provide clearer views. Traditional mammograms take two flat images per breast, while 3D mammograms (also called digital breast tomosynthesis) capture multiple images from various angles, offering more detail. Typically, 2D mammograms are used for standard screenings, while 3D mammograms are recommended for patients with higher risk factors or specific needs that require more detailed imaging.
When additional or more thorough imaging is needed, there are other methods to assess breast health:
A biopsy is the definitive diagnostic test for breast cancer. While medical imaging can detect abnormalities, lumps and growths, a biopsy is the method used to determine if these cells are cancerous. While being told you need a breast biopsy can be stressful, it’s important to remember that most biopsies end up being benign.
During the procedure, a doctor uses a long, thin needle to collect a tissue sample from the breast for analysis. There are different biopsy methods, depending on factors such as the size of the sample needed and other considerations. Some biopsies are even guided by MRI or ultrasound to target the suspicious area more accurately.
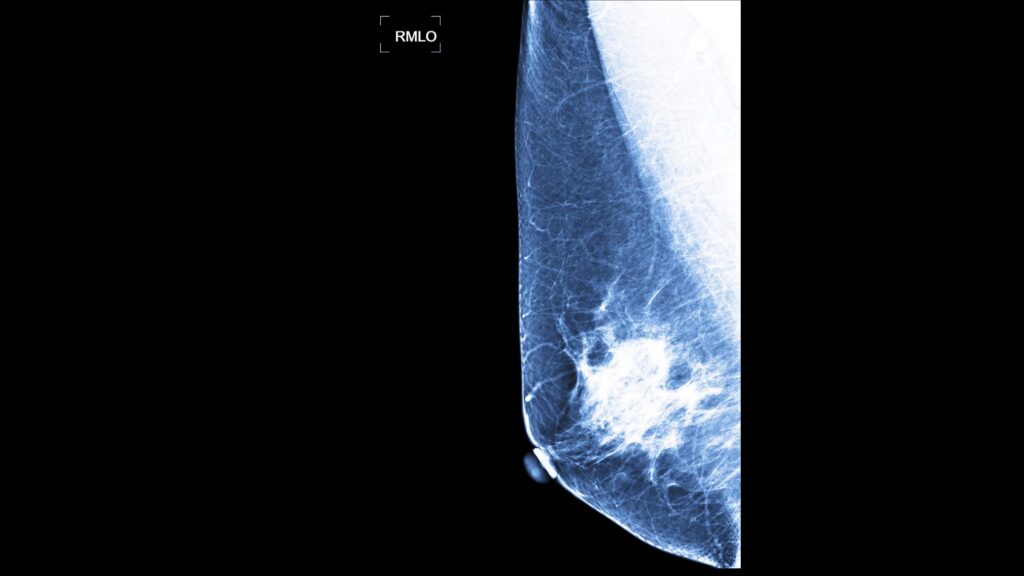
Mammogram showing BI-RADS level two which is a benign finding
Breast imaging results are often indicated by a BI-RADS score, short for Breast Imaging Reporting and Data System. The scale ranges from 0 to 6, with each score providing a different level of indication:
Breast cancer staging is helpful for prognosis and treatment decisions. The staging depends on tumor location and size, if it has spread and the type of cancer it is. Here are the stages:
It hasn’t spread from the patient’s breast ducts to other breast tissue so it is considered noninvasive. It is the easiest stage to treat.
Cancer cells have spread to adjacent breast tissue:
A tumor or tumors have formed from the cancerous cells:
Some possibilities for stage 3:
Stage 4 can mean:
The breast cancer grading system is different from the staging system. It indicates how quickly cancer cells are growing and how much they differ from normal tissue cells. While grading doesn’t determine a patient’s treatment plan on its own, it plays a significant role in deciding the next steps:
It’s important to remember that the grade alone isn’t an indication of cancer severity. For example, a patient can have stage 1 breast cancer that is classified as grade 3. Grading is simply a measure of how quickly the cancer is progressing, which may influence the timing of the treatment plan. The grade doesn’t necessarily affect prognosis.
There are a variety of treatments for breast cancer, including:
Your breast imaging results are interpreted by a radiologist—an expert in medical imaging—who carefully reviews your scans and provides a detailed report of any findings. This report is then sent to your referring physician, who, with a deeper understanding of your medical history and past exams, can offer further insights and recommendations on next steps in a follow-up appointment.
Turnaround times for imaging results can vary widely depending on the facility and your doctor’s availability. Often, patients wait a week or more and receive their results during a follow-up appointment. With PocketHealth, your imaging results are securely accessible as soon as they’re approved for release by the hospital or imaging clinic. This allows you the opportunity to review your results and prepare questions ahead of your follow-up visit.
When you do receive your reports, it’s common to find medical terminology confusing. To help you better understand your breast imaging results, PocketHealth provides clear definitions and illustrations for complex medical terms—plus an in-depth explanation of your full imaging report. This is paired with highlights of key anatomy in your imaging to help you better comprehend what you’re looking at.
Here are some common questions regarding breast cancer diagnosis.
While imaging helps identify abnormalities and tumors, it cannot definitively determine if a tumor is cancerous. In cases of benign cysts or calcifications, imaging can often rule out cancer without further testing. However, if the growth is less clear, a biopsy is the only reliable way to confirm whether it is cancerous. That said, most tumors that are biopsied turn out to be benign.
There isn’t a blood test that can outright detect breast cancer, but they can be useful for assessments. A tumor marker blood test may detect proteins produced by cancer cells, which could suggest the presence of a tumor. However, high levels of these markers do not necessarily confirm cancer, and some cancers do not produce these markers at all. Therefore, this test is a helpful supplement to diagnostic imaging and biopsies, but it should not be relied on as the sole method of diagnosis.
Similarly, patients can be tested for gene mutations (such as BRCA1 and BRCA2) that may increase their risk of developing breast cancer. However, this test does not provide a diagnosis, and individuals with these mutations may never develop the disease.
There are several factors that can increase a patient’s risk for breast cancer, but it’s important to remember that these don’t necessarily mean the disease will develop. Here are some known factors:
The general breast screening recommendation is that AFAB patients with normal risk factors have a mammogram every other year from the ages of 40 to 74. High-risk patients may be advised to have their screenings more frequently or at an earlier age. This may vary by state or province.
If you’re located in Ontario, you’ll also have the option to get your breast cancer risk score and determine your eligibility for Ontario Breast Screening Program (OBSP), as part of PocketHealth’s suite of breast health tools. If you’re eligible for OBSP, you can even book your next mammogram directly through PocketHealth.
If you are experiencing a breast cancer diagnosis, just know that you’re not alone. It is the second most common cancer type for U.S. based AFAB patients, with skin cancer being the first. Also, it may be helpful to remember that breast cancer is one of the most intensely studied and prioritized medical conditions. New research and treatments progress regularly. Additionally, the current overall average survival rate for breast cancer patients is 91%. Lastly, there are several support groups and resources that may help you through this stressful time, including:
Given the routine nature of breast imaging, tracking changes over time is essential. PocketHealth provides easy access to all your breast imaging records in one place, allowing you to be actively involved in your health journey. All of your images and reports are permanently available in one secure location and can be accessed online—anytime, anywhere. Reports can also be easily shared with other members of your care team, and you can even print and store these reports for your own use. When used in conjunction with your medical provider’s professional advice, it is a powerful tool to better understand your imaging results.
PocketHealth also provides personalized health insights based on the findings in your report to help you stay on top of any next steps. This includes clearly surfacing any follow-up actions found in your report and generating customized questions to ask your doctor so you can make the most of your follow-up appointment. For Mary, accessing her breast imaging through PocketHealth helped her catch the medical recommendation for more frequent mammogram screenings, something her clinic had missed.
While a breast cancer diagnosis is overwhelming, better understanding your results and working closely with your healthcare team can give you the best chance of managing your diagnosis and further protecting your health.
Published: February 12, 2025
Trusted by more than 900+ hospitals and clinics.